Pain that intensifies when sitting down can be more than just a nuisance: consult in time.
Perianal abscess is one of the most frequent emergencies in proctology. Although it may appear to be a minor localised infection, if not treated in time it can lead to painful complications and chronic recurrences. Identifying it quickly and acting decisively is key to avoiding sequelae such as anal fistulas.
What is a perianal abscess and why does it form?
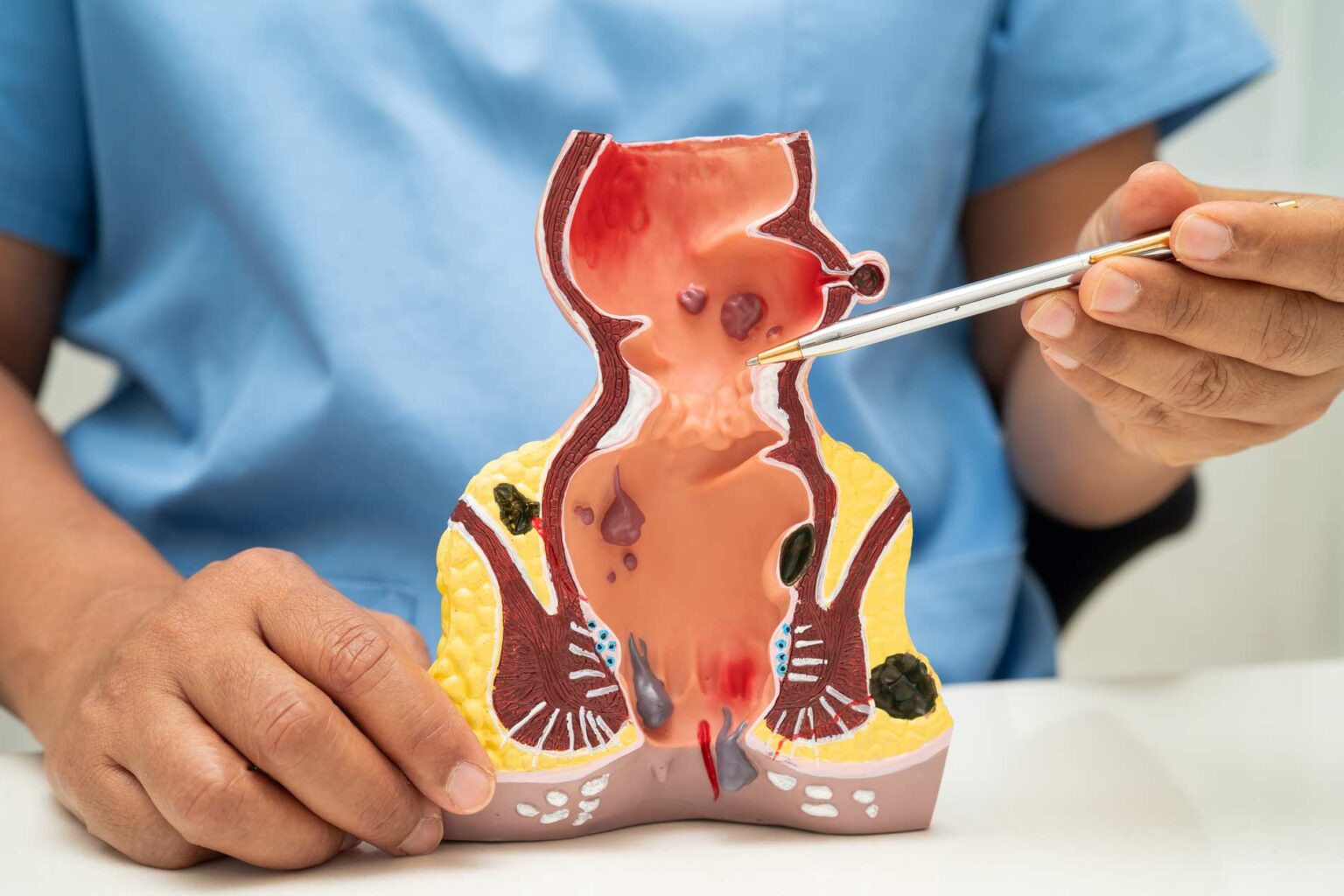
A perianal abscess is a accumulation of pus in the tissues near the anus and rectumThe infection is caused by an infection in the anal glands leading to the anal canal.
These normally inconspicuous glands can become clogged and give rise to a small pocket of infection. If the bacteria multiply, the infection progresses and a purulent collection forms. This causes pain, redness and swelling in the area, and can make it difficult to perform such basic functions as sitting, walking or going to the toilet.
Risk factors:
- Chronic constipation or excessive straining.
- Inflammatory bowel disease (especially Crohn's disease).
- Diabetes mellitus.
- Trauma, microcracks or previous interventions in the area.
- Immunosuppression.
Main symptoms of perianal abscess
Symptoms develop in the form of fast and intense:
- Acute and throbbing pain in the anal area, which is worse when sitting, walking or defecating.
- Visible inflammation in the form of a hard, red, warm lump near the anus.
- Fever and general malaise (in more advanced cases).
- Difficulty or fear of defecation by pain.
- In some cases, spontaneous discharge of pus if the abscess drains on its own.
The presence of these signs is reason enough for consultation urgently with a specialist in general surgery or proctology.
What is the difference between an abscess and an anal fistula?
- The perianal abscess is an acute, localised infection. It may resolve completely if properly drained.
- The anal fistula is a chronic complication which occurs when, after the abscess, a small duct forms that connects the inside of the anus to the perianal skin. Pus or fluid may continue to drain out of this passage over time.
It is estimated that up to 50% of abscesses end up generating a fistula if they are not treated correctly or if there are predisposing factors.
Treatment: antibiotic or surgery?
Although some mild cases may be accompanied by antibiotic treatment, the majority of perianal abscesses require urgent surgical drainage.. The surgery consists of:
- Make a small incision over the abscessed area to drain the pus.
- Cleaning of the infected area and occasional placement of a gauze pad (wick).
- Sometimes the wound is left open to allow progressive drainage.
It is a short, safe, outpatient procedure in most cases. Pain relief is immediate after evacuation of the pus.
Exclusive use of antibiotics is often not enoughexcept in immunosuppressed patients, with extensive cellulitis or high fever without a well-defined collection.
When is scheduled surgery required?
Once the acute infection has been controlled, if the patient has persistent symptoms or a secondary anal fistula develops, elective surgery may be necessary to resolve the root of the problem.
Indications for planned surgery:
- Persistent discharge from an opening in the skin.
- Recurrence of the abscess in the same area.
- Diagnosis of anal fistula by examination or endoanal ultrasound.
- Complex fistulae (curves, multiple paths, sphincter relationship).
Surgical techniques vary according to the type of fistula: fistulotomy, placement of fishing lines, LIFT, flaps, etc. The aim is to heal the fistula without damaging continence.
Conclusion
A perianal abscess is more than a painful "pimple": it is an emergency that requires prompt medical assessment. With proper treatment and subsequent follow-up, progression to fistula and associated chronic discomfort can be avoided.